During an emergency or at the end of life, you may face questions about their medical treatment and not be able answer them. You may assume your loved ones know what you would want, but that’s not always true. In one study, people guessed nearly one out of three end-of-life decisions for their loved one incorrectly.
Research shows that you are more likely to get the care you want if you have conversations about your future medical treatment and put a plan in place. It may also help your loved ones grieve more easily and feel less burden, guilt, and depression.
What is advance care planning?
Advance care planning involves discussing and preparing for future decisions about your medical care if you become seriously ill or unable to communicate your wishes. Having meaningful conversations with your loved ones is the most important part of advance care planning. Many people also choose to put their preferences in writing by completing legal documents called advance directives.
Advance Care Planning: A Conversation Guide
Want to learn more about advance care planning? NIA's guide offers conversation Tips, worksheets, and more.
What are advance directives?
Advance directives are legal documents that provide instructions for medical care and only go into effect if you cannot communicate your own wishes.
The two most common advance directives for health care are the living will and the durable power of attorney for health care.
- Living will: A living will is a legal document that tells doctors how you want to be treated if you cannot make your own decisions about emergency treatment. In a living will, you can say which common medical treatments or care you would want, which ones you would want to avoid, and under which conditions each of your choices applies. Learn more about preparing a living will.
- Durable power of attorney for health care: A durable power of attorney for health care is a legal document that names your health care proxy, a person who can make health care decisions for you if you are unable to communicate these yourself. Your proxy, also known as a representative, surrogate, or agent, should be familiar with your values and wishes. A proxy can be chosen in addition to or instead of a living will. Having a health care proxy helps you plan for situations that cannot be foreseen, such as a serious car accident or stroke. Learn more about choosing a health care proxy.
Think of your advance directives as living documents that you review at least once each year and update if a major life event occurs such as retirement, moving out of state, or a significant change in your health.
Who needs an advance care plan?
Advance care planning is not just for people who are very old or ill. At any age, a medical crisis could leave you unable to communicate your own health care decisions. Planning now for your future health care can help ensure you get the medical care you want and that someone you trust will be there to make decisions for you.
Advance care planning for people with dementia
Many people do not realize that Alzheimer’s disease and related dementias are terminal conditions and ultimately result in death. People in the later stages of dementia often lose their ability to do the simplest tasks. If you have dementia, advance care planning can give you a sense of control over an uncertain future and enable you to participate directly in decision-making about your future care. If you are a loved one of someone with dementia, encourage these discussions as early as possible. In the later stages of dementia, you may wish to discuss decisions with other family members, your loved one’s health care provider, or a trusted friend to feel more supported when deciding the types of care and treatments the person would want.
What happens if you do not have an advance directive?
If you do not have an advance directive and you are unable to make decisions on your own, the state laws where you live will determine who may make medical decisions on your behalf. This is typically your spouse, your parents if they are available, or your children if they are adults. If you are unmarried and have not named your partner as your proxy, it’s possible they could be excluded from decision-making. If you have no family members, some states allow a close friend who is familiar with your values to help. Or they may assign a physician to represent your best interests. To find out the laws in your state, contact your state legal aid office or state bar association.
Will an advance directive guarantee your wishes are followed?
An advance directive is legally recognized but not legally binding. This means that your health care provider and proxy will do their best to respect your advance directives, but there may be circumstances in which they cannot follow your wishes exactly. For example, you may be in a complex medical situation where it is unclear what you would want. This is another key reason why having conversations about your preferences is so important. Talking with your loved ones ahead of time may help them better navigate unanticipated issues.
There is the possibility that a health care provider refuses to follow your advance directives. This might happen if the decision goes against:
- The health care provider’s conscience
- The health care institution’s policy
- Accepted health care standards
In these situations, the health care provider must inform your health care proxy immediately and consider transferring your care to another provider.
Other advance care planning forms and orders
You might want to prepare documents to express your wishes about a single medical issue or something else not already covered in your advance directives, such as an emergency. For these types of situations, you can talk with a doctor about establishing the following orders:
- Do not resuscitate (DNR) order: A DNR becomes part of your medical chart to inform medical staff in a hospital or nursing facility that you do not want CPR or other life-support measures to be attempted if your heartbeat and breathing stop. Sometimes this document is referred to as a do not attempt resuscitation (DNR) order or an allow natural death (AND) order. Even though a living will might state that CPR is not wanted, it is helpful to have a DNR order as part of your medical file if you go to a hospital. Posting a DNR next to your hospital bed might avoid confusion in an emergency. Without a DNR order, medical staff will attempt every effort to restore your breathing and the normal rhythm of your heart.
- Do not intubate (DNI) order: A similar document, a DNI informs medical staff in a hospital or nursing facility that you do not want to be on a ventilator.
- Do not hospitalize (DNH) order: A DNH indicates to long-term care providers, such as nursing home staff, that you prefer not to be sent to a hospital for treatment at the end of life.
- Out-of-hospital DNR order: An out-of-hospital DNR alerts emergency medical personnel to your wishes regarding measures to restore your heartbeat or breathing if you are not in a hospital.
- Physician orders for life-sustaining treatment (POLST) and medical orders for life-sustaining treatment (MOLST) forms: These forms provide guidance about your medical care that health care professionals can act on immediately in an emergency. They serve as a medical order in addition to your advance directive. Typically, you create a POLST or MOLST when you are near the end of life or critically ill and understand the specific decisions that might need to be made on your behalf. These forms may also be called portable medical orders or physician orders for scope of treatment (POST). Check with your state department of health to find out if these forms are available where you live.
You may also want to document your wishes about organ and tissue donation and brain donation. As well, learning about care options such as palliative care and hospice care can help you plan ahead.
How can you get started with advance care planning?
To get started with advance care planning, consider the following steps:
- Reflect on your values and wishes. This can help you think through what matters most at the end of life and guide your decisions about future care and medical treatment.
- Talk with your doctor about advance directives. Advance care planning is covered by Medicare as part of your annual wellness visit. If you have private health insurance, check with your insurance provider. Talking to a health care provider can help you learn about your current health and the kinds of decisions that are likely to come up. For example, you might ask about the decisions you may face if your high blood pressure leads to a stroke.
- Choose someone you trust to make medical decisions for you. Whether it’s a family member, a loved one, or your lawyer, it’s important to choose someone you trust as your health care proxy. Once you’ve decided, discuss your values and preferences with them. If you’re not ready to discuss specific treatments or care decisions yet, try talking about your general preferences. You can also try other ways to share your wishes, such as writing a letter or watching a video on the topic together.
- Complete your advance directive forms. To make your care and treatment decisions official, you can complete a living will. Similarly, once you decide on your health care proxy, you can make it official by completing a durable power of attorney for health care.
- Share your forms with your health care proxy, doctors, and loved ones. After you’ve completed your advance directives, make copies and store them in a safe place. Give copies to your health care proxy, health care providers, and lawyer. Some states have registries that can store your advance directive for quick access by health care providers and your proxy.
- Keep the conversation going. Continue to talk about your wishes and update your forms at least once each year or after major life changes. If you update your forms, file and keep your previous versions. Note the date the older copy was replaced by a new one. If you use a registry, make sure the latest version is on record.
Everyone approaches the process differently. Remember to be flexible and take it one step at a time. Start small. For example, try simply talking with your loved ones about what you appreciate and enjoy most about life. Your values, treatment preferences, and even the people you involve in your plan may change over time. The most important part is to start the conversation.
How to find advance directive forms
You can establish your advance directives for little or no cost. Many states have their own forms that you can access and complete for free. Here are some ways you might find free advance directive forms in your state:
- Contact your State Attorney General’s Office.
- Contact your local Area Agency on Aging. You can find your area agency phone number by visiting the Eldercare Locator or by calling 800-677-1116.
- Download your state’s form online from one of these national organizations: AARP, American Bar Association, or National Hospice and Palliative Care Organization.
- If you are a veteran, contact your local Veteran's Affairs (VA) office. The VA offers an advance directive specifically for veterans.
Some people spend a lot of time in more than one state. If that's your situation, consider preparing advance directives using the form for each state, and keep a copy in each place, too.
Do you need a lawyer to create advance directives?
Not necessarily. A lawyer can help but is not required to create your advance directives. However, if you have a lawyer, you should give them a copy of your advance directive. If you need help with planning, contact your local Area Agency on Aging. Other possible sources of legal assistance and referral include state legal aid offices, state bar associations, and local nonprofit agencies, foundations, and social service agencies.
There are also organizations that enable you to create, download, and print your forms online, but they may charge fees. Before you pay, remember there are several ways to get your forms for free. Some free online resources include:
- PREPARE for Your Care: An interactive online program that was funded in part by NIA. It is available in English and Spanish.
- The Conversation Project: A series of online conversation guides and advance care documents available in English, Spanish, and Chinese. The Conversation Project is a public engagement initiative led by the Institute for Healthcare Improvement.
If you use forms from a website, check to make sure they are legally recognized in your state. You should also make sure the website is secure and will protect your personal information. Read the website’s privacy policy and check that the website link begins with “https” (make sure it has an “s”) and that it has a small lock icon next to its web address.
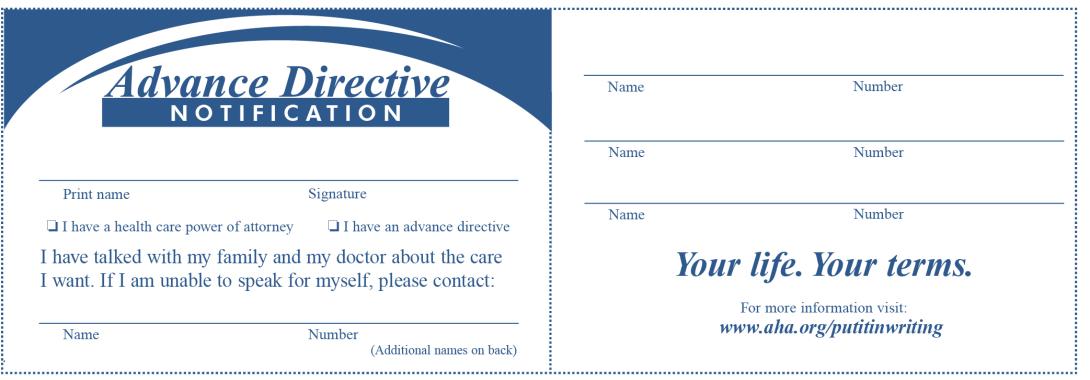
Some people also choose to carry a card in their wallet indicating they have an advance directive and where it is kept. Below is an example from the American Hospical Association.
You may also be interested in
- Finding out more about choosing a health care proxy
- Learning about legal and financial planning for people with dementia
- Reading about preparing a living will
For more information about advance directives
Administration for Community Living (ACL)
202-401-4634
www.acl.gov
Department of Veterans Affairs
877-222-8387
www.va.gov/geriatrics
OrganDonor.gov
Health Resources & Services Administration
www.organdonor.gov
American Bar Association
800-285-2221
www.americanbar.org
CaringInfo
National Hospice and Palliative Care Organization
800-658-8898
www.caringinfo.org
The Conversation Project
866-787-0831
www.theconversationproject.org
National POLST
202-780-8352
www.polst.org
PREPARE for Your Care
www.prepareforyourcare.org
Create your own plan
NIA’s new email series, Ready, Set, Plan! A Weekly Guide to Advance Care Planning, will help you start planning for your future health care over seven weeks. Sign up today!
